I have this conversation all too often with people. “My employer is making me get the flu shot or they will fire me. Why do they do that?”
Good Intentions
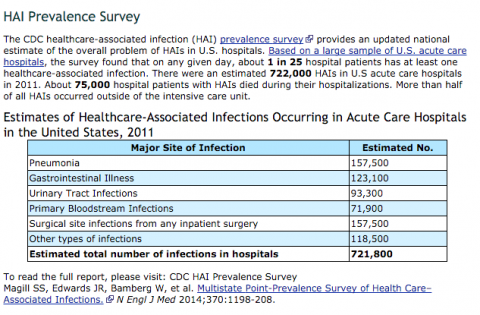
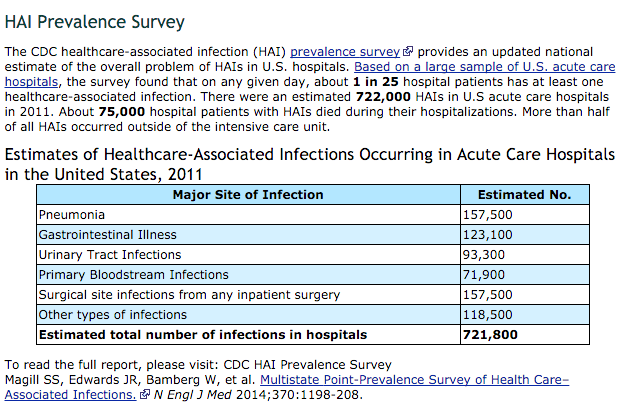
Why do they force you to get a flu shot? Most often it’s a hospital setting and the hospital doesn’t want transmission of a virus to the people that have a compromised immune system. Hospital acquired infections is a sad reality. In 2011, there was an estimated 721,800 infections acquired from inside the hospital. That translates to an infection rate of 1 out of every 25 hospital patients. 75,000 of the 722,000-ish infections lead to death. The person came to the hospital for one reason but then died due to acquiring an infection within the hospital walls.
This isn’t to poo poo the hospitals. You go the hospital when you’re sick. Your immune system is already tanked and now you’re exposed to a host of other sick people. I’m sure hospitals do the best they can at preventing transmission of infectious disease.
One of those ‘good intention’ strategies is to require a flu shot for any hospital employee, even if you don’t take care of patients directly.
Sad Reality
The sad reality is that it doesn’t work. For one, the flu shot hasn’t been proven effective in those with lower immunity. There was an INCREASE in flu-related deaths from 1980 to 2001, when vaccine coverage went from 15-20% coverage to over 65% coverage. Yet, the flu shot is recommended every year.
Since it doesn’t work in the immune compromised, then all the people around them ‘need to get the flu shot to protect them.’ Again, good intentions with a sad reality.
There are over 200 viruses that cause the flu and flu-like illness that produce the exact same ‘Influenza-Like Illness (ILI)’ symptoms (fever, headache, aches, pains, cough and runny noses). Without laboratory tests, doctors cannot tell the two illnesses apart. Both last for days and rarely lead to death or serious illness. At best, vaccines might be effective against only influenza A and B, which represent about 10% of all circulating viruses.
The Cochran Library took 90 reports of 116 studies in 2013 and compared the effect of influenza vaccine with placebo or no intervention. Sixty-nine reports were clinical trials (over 70,000 people), 27 were comparative cohort studies (about eight million people) and 20 were case-control studies (nearly 25,000 people). Of the 116 studies, 23 (three case-control and 20 cohort studies) were performed during pregnancy (about 1.6 million mother-child couples).
The preventive effect of parenteral inactivated influenza vaccine on healthy adults is small: at least 40 people would need vaccination to avoid one ILI case and 71 people would need vaccination to prevent one case of influenza . Their conclusion is that vaccination shows no appreciable effect on working days lost or hospitalization.
The same authors of this review from back in 2010 assessed all trials that compared vaccinated people with unvaccinated people. The combined results of these trials showed that under ideal conditions (vaccine completely matching circulating viral configuration) 33 healthy adults need to be vaccinated to avoid one set of influenza symptoms. In average conditions (partially matching vaccine) 100 people need to be vaccinated to avoid one set of influenza symptoms.
Vaccine use did not affect the number of people hospitalized or working days lost but caused one case of Guillian-Barré syndrome (a major neurological condition leading to paralysis) for every one million vaccinations. Fifteen of the 36 trials were funded by vaccine companies and four had no funding declaration. Our results may be an optimistic estimate because company-sponsored influenza vaccines trials tend to produce results favorable to their products and some of the evidence comes from trials carried out in ideal viral circulation and matching conditions and because the harms evidence base is limited.
In other words, it does little to nothing in preventing transmission and little to nothing to prevent lost days from work and little to nothing to prevent hospitalizations. Despite all this evidence, you’re going to see any and all media reports end their article with “the flu shot is still the most effective way at preventing the flu.”
Even last year’s reports say that flu shot was only 18% effective. The placebo consistently gets 33% of the population. You can get the flu shot or not, I don’t care. Maybe you’re in the 33% of placebo users that got great results with believing it worked or maybe you’re in the 18% that it was actually effective and happy with your results. When I start caring is when it starts being forced on people with no evidence that it will accomplish less sick days, less hospitalizations, and less transmission.
To answer the question, “why does my work make me get the flu shot?” All I can say is, “I don’t know.”


The medical industry’s philosophy is one of combined ego of “medicine works”, even when there is little or no proof or evidence. If you do not believe that to be true, perhaps you are just not suited to be part of the medical industry. Look at all the failures of the past and the medical attitude toward those failures if you have doubts. But then what do I know?
Being in healthcare, I can tell you the real reason they are mandating vaccination. It all comes down to money. Thanks to the government, if hospitals don’t have a certain percent of employees vaccinated, their reimbursement is cut. Before this new requirement there were no forced vaccinations