
If you were a child of the 80s and 90s like myself, you will remember this commercial. “This is your brain. This is drugs. This is your brain on drugs. Any questions?”
With the ever rising incidences and diagnoses for ADHD, Autism, Depression, Parkinson’s, and Alzheimer’s and nothing to resolve them in the medical world, I think we can change the 80s drug slogan to make it more applicable for today. After all, the more we ‘early diagnose and manage/treat’ a condition, the more disability associated with that condition rises. The best case scenario your doctor provides is to ‘manage’ the symptoms.
But here’s the reality. Symptoms aren’t stupid. Your body never does anything stupid. Symptoms are nothing more than your attempts at buying time to escape what is potentially dangerous or harmful. That potential danger could be something you ate, a lack of movement, a poor relationship, or chemical influence. One of those symptoms is inflammation, regardless of the condition or disease process.
“This is your brain. This is inflammation. This is your brain on inflammation. Any questions?”
If there’s a commonality of brain inflammation to all these mental/emotional conditions, then how does the brain get inflamed? Don’t think of inflammation as an isolated event. Inflammation is a byproduct of an immune response due to trauma. And again, don’t look at trauma as just an event. Trauma is a persistent pattern of dysfunction. It could be physical, chemical, or emotional/social/spiritual.
Our immune system (inflammation) gets activated for 2 main reasons.
- Fight Infection and be used as a first line defense. The coughing, sneezing, runny nose, diarrhea, fever, and sweating during a flu isn’t the fault of the bug. This is your body’s response to the bug. You sneeze to expel the bug at 35 mph to a distance of 12-20 feet away. Suppressing these symptoms with steroids, anti-histamines, and other amphetamine based cold and cough meds makes you feel better while allowing the little buggers to stick around longer, keeping you sick longer. You took away your defenses (symptoms).
- Injury/Tissue Repair. This could be a car accident, concussion, you name it. But it’s the same as working out. You work out to get bigger and stronger. You are voluntarily injuring yourself for the purpose of allowing your body to build it back up again. All that soreness you experience the day or 2 after a workout isn’t a build of lactic acid. It’s the damage you created in your workout. You sliced and diced your cells. Inflammation comes in to clean up the debris and recruit factors to rebuild. Taking prescription anti-inflammatory compounds like NSAIDS delays your healing and recovery. You may feel better all while wondering why you keep getting re-injured.
In either scenario, there is a push within the body to recover. One of those major recovery molecules is glutathione. In order for your body to make glutathione, there are a series of conversion steps, in which one of those is the production and conversion of homocysteine. We need homocysteine but it becomes a problem when it gets too high or too low. Elevations in homocysteine have major links to cardiac and cognitive damage.
What can elevated homocysteine do? It can break down the blood brain barrier. This sets the stage for things that shouldn’t be allowed in the brain to enter in. And when there’s an unwelcome guest in your house, it gets attacked.
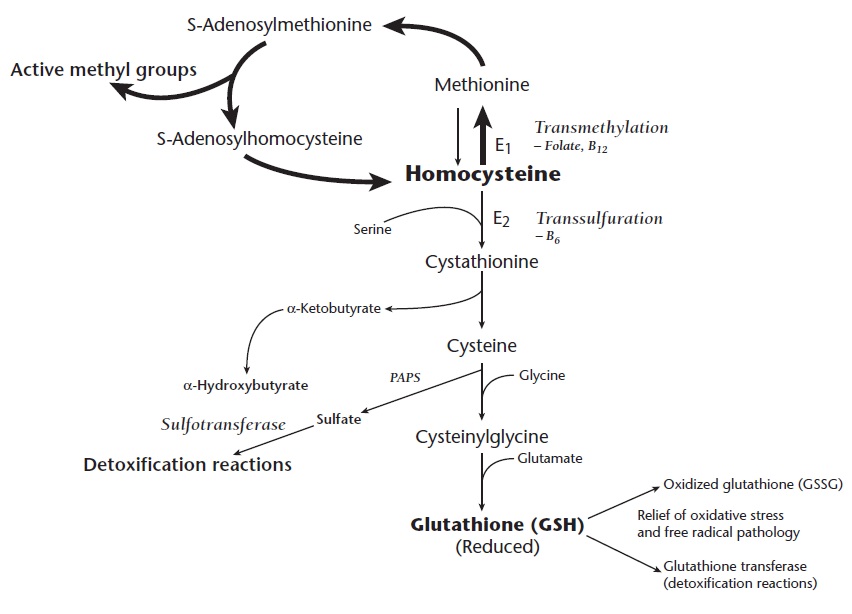
Something you may notice in the chart are key nutrients like folate, B12, and B6. All are essential in the process of homocysteine utilization. What does a lack in these nutrients (or an inability to process these nutrients) have in common with symptoms of brain inflammation like depression, dementia, and Parkinson’s? Pretty much everything. The symptoms of B12 deficeincy look virtually identical to brain inflammation. And brain inflammation looks identical to depression, anxiety, ADHD, and the gambit. But don’t just go load up on B12 yet.
So what’s the point?
You could use homocysteine levels as a risk factor for brain inflammation and potential blood brain barrier breakdown, leading to depression, anxiety, Alzheimer’s, and Parkinson’s; But there’s something you can do to assess if you have a compromised blood brain barrier right now and at home.
Blood Brain Barrier Assessment
This needs to be set up a bit. Amino acids (basic protein, enzyme, hormone, and neurotransmitter building blocks) can cross from the body to the brain through the blood brain barrier. One of the main reasons is to interact with the HPA (Hypothalamus-Pituitary-Adrenal) axis. This is important to save your life when it perceives danger. There are 6 common neurotransmitters that are major players in this pathway: Serotonin, Dopamine, Norepinephrine, Epinephrine, GABA, and Glutamate.
All of these will cross the blood brain barrier, EXCEPT GABA. It’s too big. Size matters.
Glutamate is the primary neurotransmitter that gets us excited. GABA is the major inhibitory neurotransmitter. It should help us relax and sleep. GABA is produced from Glutamate with a little help from P-5-P (the active form of B6).
SIDE NOTE #1: Glutamate is just a string of folic acid molecules. If a person cannot process folic acid well (MTHFR), there is potential that folic acid gets broken down into glutamate, instead of supporting the homocysteine/glutathione cycle. While glutamate can convert to GABA, it can also convert to dopamine and you just slammed your foot on the car accelerator. Take home point, be careful of your fortified folic acid consumption. What may’ve good intentions may actually have unintended consequences of accelerating brain excitation (hello brain inflammation).
 SIDE NOTE #2: Glutamate can become GABA (inhibitory), or aspartate (excitatory and, in excess, neurotoxic). Ketogenic diets seem to favor glutamate becoming GABA rather than aspartate. No one knows exactly why, but part of the reason has to do with how ketones are metabolized, and how ketosis favors using acetate (acetoacetate is one of the ketone bodies, after all) for fuel. Acetate becomes glutamine, an essential precursor for GABA. Glutamine is also repair tool for the gut.
SIDE NOTE #2: Glutamate can become GABA (inhibitory), or aspartate (excitatory and, in excess, neurotoxic). Ketogenic diets seem to favor glutamate becoming GABA rather than aspartate. No one knows exactly why, but part of the reason has to do with how ketones are metabolized, and how ketosis favors using acetate (acetoacetate is one of the ketone bodies, after all) for fuel. Acetate becomes glutamine, an essential precursor for GABA. Glutamine is also repair tool for the gut.
Is Your Brain Leaking? GABA Challenge.
Here’s the self assessment. Just a warning. The point of this test is to make you feel weird. It’s called the GABA Challenge Test. Remember, GABA should slow us down. And there are many drugs that try and mimic GABA’s effects. GABA and its derivatives are often used to treat things like anxiety, seizures and it acts as a sedative or a muscle relaxant. Alcohol and Valium are probably the most recognized GABA stimulators. But taking GABA directly should have ZERO effect on your system since it cannot cross the blood brain barrier. If that barrier is intact, you should feel absolutely nothing.
DIRECTIONS and my introduced to this test come to us from Dr. Robert Luckey (you can call him Bobby).
- About 1-2 hours after dinner, on a night that you have nothing planned, take 1000 mg of GABA. You can find this pretty cheap at a health food store. It’s cheap because it’s absolutely useless. It should do NOTHING!
- Notice any unusual slowing down type feelings, ranging from drunken to lethargy, or simply slowed down.
- Notice any excitation, agitation, or other stimulation such as feeling wired, which will happen in approximately 20% of the cases of compromised BBB. Most will feel inhibited.
- Go to bed. If you are slowed, it will be gone by the morning. If you feel hung over in the morning, the process of neurodegeneration is more advanced, and requires significant attention.
- ANY change, excitation or inhibition is a positive test for damage to the Blood Brain Barrier.
Remember, you should feel NOTHING by taking GABA. If you are taking supplements with GABA in them and you feel fantastic or they help you sleep, you have some major issues happening. Or it could be some of the other ingredients in the supplement helping. In any scenario, GABA is a waste of your money. For my clients that want to try this, we have some GABA for you at the office.
If you have any change, the next steps are to find the main sources of inflammation. Is there an auto-immune condition or persistent infections? Do you have unresolved emotional trauma (persistent patterns of dysfunction) from your childhood? Do you have genetic variances? Or do you just plain and simple have a crappy lifestyle. If you want help, you know how to find me.


4 Comments